Monkeypox has recently raised public concern after appearing in regions where it was once rare. While it’s similar to smallpox, it’s usually milder and less contagious. Knowing the facts can help ease fear and improve outbreak response.
What Is Monkeypox?
Monkeypox is a rare viral infection that causes fever, rash, and skin lesions. It is similar to smallpox but is less severe and less contagious overall. The disease, though uncommon, can spread from animals to humans and occasionally from person to person through close contact.
History of Monkeypox
The virus was first discovered in 1958 after outbreaks in laboratory monkeys, which is how the disease got its name. However, monkeys are not the primary carriers. Rodents and small mammals are believed to be the main animal hosts.
The First Human Case
The first recorded human case of monkeypox happened in 1970 in the Democratic Republic of Congo (DRC).
The patient was a 9-month-old boy named Zaire, who lived in a remote village. He developed a rash similar to smallpox, but tests later confirmed it was monkeypox. Sadly, the boy died a few days after diagnosis. His case raised international concern because smallpox was in decline, yet a similar virus had appeared in humans.
This case marked the beginning of monkeypox as a recognized human disease.
How does Monkeypox spread?
Monkeypox spreads through:
- Direct contact with infected animals or people
- Contact with body fluids, skin lesions, or respiratory droplets
- Touching contaminated objects such as bedding or clothing
Human-to-human transmission generally requires prolonged close contact, often within households, healthcare settings, or through shared personal items.
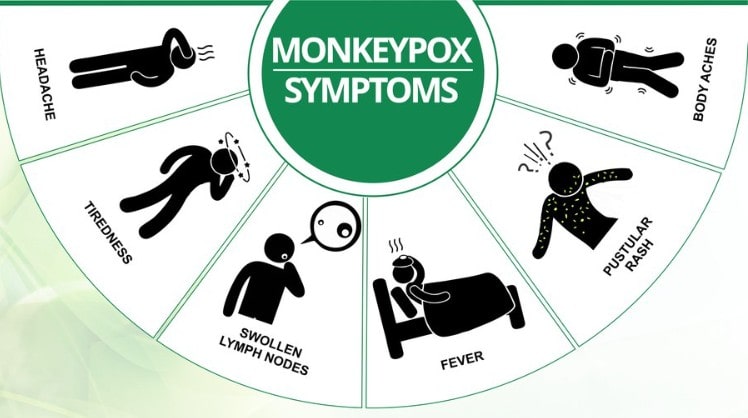
Symptoms of Monkeypox
Monkeypox is a viral illness that can cause flu-like symptoms and a skin rash within 5 to 21 days of exposure. Early detection helps stop its spread.
Early Phase Symptoms:
In the initial stage, people often experience flu-like symptoms that can make them feel very unwell.
Common early signs include:
- Fever: One of the first signs to develop, often sudden and high.
- Severe headache: Persistent and can be quite intense.
- Muscle aches: Body-wide discomfort, especially in the back and legs.
- Fatigue: A deep sense of tiredness and weakness.
- Swollen lymph nodes: This is a key symptom that sets monkeypox apart from diseases like smallpox and chickenpox.
Note: Swollen lymph nodes are an important clue for doctors to distinguish monkeypox from other similar viral infections.
Rash Development and Progression
After flu-like symptoms, a rash usually appears, starting on the face and spreading to the palms, soles, chest, back, and sometimes the genitals. It progresses through distinct stages.
Rash Stages:
- Flat red spots: Often the first visible skin change.
- Raised bumps: The spots become more solid and elevated.
- Fluid-filled blisters: The bumps fill with clear fluid.
- Pus-filled lesions: The blisters fill with yellowish pus.
- Scabs: The lesions dry out, forming scabs that eventually fall off.
Additional Notes on the Rash
- The rash can be itchy or painful as it progresses through its stages.
- The number of skin lesions can vary significantly, from just a few spots to widespread coverage.
- In some cases, the rash can cover large areas of the body, leading to increased discomfort and sensitivity.
What are the Causes of Monkeypox?
Monkeypox is caused by the monkeypox virus, which can spread from animals to humans and occasionally from person to person. Although it is a zoonotic disease, meaning it originates in animals, the virus can quickly move between humans through close contact.
Sources of Infection
Animal-to-Human Transmission
People can get monkeypox by directly touching infected animals, especially rodents(rats, mice, and squirrels) and monkeys. Handling or eating bushmeat (wild animal meat) increases the risk of exposure, particularly in areas where this is common.
Human-to-Human Transmission
Monkeypox can spread between people through:
- Skin-to-skin contact with rashes or lesions
- Body fluids and respiratory droplets during close interaction
- Contaminated objects like bedding, clothing, or towels
How Is Monkeypox Treated?
There’s no cure for monkeypox, but most people recover with rest, fluids, and symptom relief. In some cases, antivirals may be used to prevent complications.
Supportive Care: Helping the Body Heal Naturally
Since monkeypox typically resolves on its own within a few weeks, supportive care is often all that’s needed to help patients through the illness. This involves simple, comforting treatments that support the body’s natural healing process.
Supportive Care Includes:
- Rest: Giving the body time and energy to fight the infection.
- Hydration: Drinking plenty of fluids to prevent dehydration, especially if fever is present.
- Pain Relief: Over-the-counter medications to reduce fever, body aches, and headaches.
- Skin Care: Gently caring for the skin and open lesions to prevent further infections and reduce scarring.
Providing emotional support and maintaining good hygiene throughout the recovery period are also important parts of care.
Antiviral Medications: For Severe Cases
In more serious cases, especially when patients have weakened immune systems or complications, doctors may recommend antiviral medications. Although these drugs were initially developed for smallpox, they show promise in treating monkeypox.
Common Antivirals Used:
- Tecovirimat (TPOXX): Often the first choice, with good results and a strong safety profile.
- Cidofovir: An antiviral that may help in severe cases but carries a risk of side effects.
- Brincidofovir: A newer option that offers potential benefits with fewer kidney-related risks than cidofovir.
These treatments are generally reserved for people with severe symptoms or those at higher risk of complications.

Is There a Vaccine for Monkeypox?
Yes, vaccines can protect against monkeypox and help control outbreaks. They work best when given before exposure but may still offer protection if taken soon after contact.
Available Vaccines:
1. JYNNEOS (Imvamune/Imvanex)
- Who: For people 18+ (sometimes used for younger in emergencies).
- Dosage: 2 doses, 28 days apart.
- Protection: Full effect 2 weeks after the second dose.
- Cost & Access: Often free or low-cost at public clinics and hospitals.
- Availability: Offline at vaccination centers.
- Safety: Very safe, with mild side effects like redness and fatigue.
2. ACAM2000
- Who: For healthy adults 18+ (not safe for everyone).
- Dosage: Single dose.
- Protection: Full effect in about 4 weeks.
- Cost & Access: Usually free but limited to emergency stockpiles.
- Availability: Only through government programs.
- Safety: Higher risk of side effects, not recommended for those with heart or immune problems.
Health authorities often recommend vaccination for people who are at higher risk of exposure, such as healthcare workers, laboratory staff, and close contacts of confirmed cases.
How to Prevent Monkeypox?
Monkeypox can be prevented by simple steps that focus on attention to personal safety, animal handling, and community hygiene practices.
Personal Prevention Tips
- Avoid close contact with individuals showing signs of monkeypox, particularly those with skin lesions or rashes
- Wash hands regularly with soap and water or use alcohol-based hand sanitizers
- Use personal protective equipment (PPE) like gloves and masks when caring for infected people
Animal Precautions
- Avoid direct contact with wild animals, especially rodents and primates
- Do not consume bushmeat or handle wild animal carcasses
- Cook all animal products thoroughly
Community-Level Prevention
- Follow public health guidelines to reduce exposure
- Support public health surveillance to detect new cases early
- Participate in vaccination programs if recommended
- Educate communities about safe animal handling and recognizing early symptoms
Public health education and timely vaccination can significantly reduce the chances of outbreaks.
Monkeypox vs. Similar Viral Infections
| Feature | Monkeypox | Chickenpox | Smallpox | HFMD | Measles | Herpes (HSV) |
|---|---|---|---|---|---|---|
| Fever | Yes (before rash) | Yes (before rash) | Yes (before rash) | Yes (mild) | Yes (before rash) | Sometimes (localized) |
| Lymph Nodes | Swollen (key sign) | Rare | Rare | No | No | No |
| Rash Spread | Face, body, extremities | Face, torso, extremities | Face, body, extremities | Hands, feet, and mouth | Face, spreads downward | Localized (mouth/genitals) |
| Rash Type | Blisters, same stage | Blisters, mixed stages | Blisters, same stage | Red spots, mild blisters | Flat red spots | Blisters or sores |
| Itching | Sometimes | Often | Sometimes | Often | Often | Yes |
| Key Difference | Lymph node swelling | Rash in mixed stages | No lymph swelling | Mild, mainly in children | Cough, runny nose, red eyes | Localized pain/sores |
Complications Associated With Monkeypox
While monkeypox is usually mild, some people may experience complications, especially if they have other health issues or a weakened immune system.
Possible Complications
- Severe skin infections
- Secondary bacterial infections
- Eye infections that can lead to vision loss
- Pneumonia
- In rare cases, encephalitis (inflammation of the brain)
- Scarring from deep skin lesions
Children, pregnant women, and people with weakened immune systems are at a higher risk of developing these complications.
Groups at Greater Risk
- Young children under the age of eight
- People with HIV or other immunodeficiencies
- Pregnant women who may pass the virus to the unborn child
Proper medical care and early treatment can help prevent these serious outcomes.
Frequently Asked Questions
Can Monkeypox Spread From Person to Person?
Yes, monkeypox can spread from one person to another through direct contact with body fluids, respiratory droplets, or skin lesions. It can also spread through contact with contaminated objects such as bedding and clothing.
Is Monkeypox a Self-Limiting Disease?
In most cases, monkeypox is self-limiting, meaning it clears up on its own within two to four weeks. People with weakened immune systems may experience more severe symptoms and require medical attention.
How Is Monkeypox Diagnosed?
Doctors usually diagnose monkeypox by examining the rash, checking for swollen lymph nodes, and reviewing the patient’s travel and exposure history. The diagnosis is confirmed through laboratory testing, such as polymerase chain reaction (PCR), which detects the monkeypox virus from skin lesion samples.
Is There a Vaccine for Monkeypox?
Yes, the JYNNEOS vaccine and the ACAM2000 vaccine can both protect against monkeypox. The JYNNEOS vaccine is generally safer and is recommended for people who may have been exposed or are at high risk, including healthcare workers.
How Can Monkeypox Outbreaks Be Controlled?
Monkeypox outbreaks can be controlled through a combination of early detection, public health surveillance, vaccination, proper hygiene practices, and community education about safe animal handling and symptom awareness.